Updated October 3, 2022.
This document seeks to address common questions about the new behavioral health provider network at AmeriHealth HMO, Inc. and AmeriHealth Insurance Company of New Jersey (collectively, AmeriHealth). It is updated regularly as additional information becomes available.
This new behavioral health network will be
effective January 1, 2023.
If you need more information or have other questions regarding the new behavioral health network, please email us at
AmeriHealthBH@amerihealth.com.
FAQ topics cover:
-
General
-
Reimbursement and Billing
-
Contracting
-
Credentialing
-
Claims
General
1) Why is AmeriHealth establishing its own network?
AmeriHealth is taking an innovative approach to behavioral health for its members that considers their entire wellness. This includes the patient's physical and behavioral health as well as equitable access to care.
We are also changing the way we work with behavioral health providers, as we work to integrate the delivery of medical and behavioral health care. We recognize the need for a closer partnership with behavioral health clinicians who treat our members, and the importance of establishing a direct and mutually beneficial relationship.
2)
Will behavioral health telemedicine continue to be offered to AmeriHealth members? If so, what is the rate?
Yes, behavioral health telemedicine will continue to be offered. The behavioral health fee schedule is the same for telehealth and in-person appointments.
3)
Will authorizations be required?
There are no planned changes to your precertification rules that exist today with Magellan. If a service does not require medical necessity review/precertification presently, it will not be required by AmeriHealth as of January 1, 2023. Requirements regarding medical necessity review/precertification do change from time to time, so please be sure to stay current with the latest updates from AmeriHealth.
Here is a link to precertification page information:
Reimbursement and Billing
4)
When will the new rates be available?
The AmeriHealth rates will be effective on January 1, 2023
5) Will the fee schedule rates change? Are the rates competitive?
We are offering a prevailing fee schedule that will be reviewed each year and, if needed, updated to reflect changes in market conditions and in consideration for Cost-of-Living Adjustments (COLA). We expect that the AmeriHealth prevailing fee schedule is an overall benefit to you and your practice, and we encourage you to participate in our network.
We recognized the need to increase the prevailing rates since our original announcement was made in October 2021. The January 1, 2023, prevailing fee schedule was updated as recently as April 2022. Please make sure you are referencing the most up to date schedule, which can be found on the PEAR portal or by emailing
AmeriHealthBH@amerihealth.com
6) Are there separate rates for HMO and PPO members? Are there different reimbursement rates?
We have simplified the fee schedule by blending the behavioral health rates. It combines PPO and HMO fees into one schedule. This means that there is one rate regardless of the member being treated. We no longer have different rates for HMO, PPO, Commercial, or Medicare Advantage members.
7) How can I access the rates?
A prevailing fee schedule of codes is included with the contract for behavioral health providers to review. The prevailing rates may change depending on a variety of factors. Regardless of when you sign the contract, your practice will receive the prevailing rates that are current as of January 1, 2023.
Providers with access to
PEAR (our provider portal) can view the most recent prevailing schedule in the Practice Management (PM) application:
- Once you log into PEAR, select PEAR PM
- Choose the Reference icon in the top right corner
- Select the Generic Fee Schedule link
For questions regarding the fee schedule:
8) Why aren't all CPT® codes included? Will they be added?
The mailed fee schedule includes the highest volume behavioral health codes that we see billed in our claims data. If codes are missing, it means that we found them to have low utilization, which do not have significant impact on overall reimbursement. If you have specific feedback concerning a required code, please send an email to
AmeriHealthBH@amerihealth.com.
9) Will the transition affect my current EFT set up?
No, if you were registered for electronic funds transfers (EFT) via Magellan, you do not need to re-register with AmeriHealth New Jersey.
If you are not currently set-up with EFT payments, or are new to AmeriHealth New Jersey as of January 1, 2023, we encourage you to register. Step-by-step instructions for registering an EFT account with AmeriHealth New Jersey can be found on our Provider News Center:
https://provcomm.amerihealth.com/archive-ah/pages/eftresources.aspx
If your effective date is January 1, 2023, when our AmeriHealth New Jersey behavioral health network goes into effect, you can still register now for electronic funds transfer (EFT) connectivity, which will show as pending until January 1, 2023.
10) How do I know what to charge members, especially those with a high deductible plan?
This process remains the same as today. Our comprehensive PEAR portal allows in-network providers to access member cost share, including co-insurance and deductible information, 24 hours a day / 7 days a week.
You may also contact our Call Center:
- AmeriHealth New Jersey: 1-888-YOUR-AH1 (1-888-968-7241)
- AmeriHealth Pennsylvania: 1-800-275-2583
11) Will there be new claims processing procedures?
Claims processing will remain the same, since claims were sent directly to AmeriHeatlh under the Magellan network.
Clinicians who furnish both medical services and behavioral health services must remember to bill with the appropriate taxonomy codes for the services rendered. This ensures that your claim is routed to the appropriate member benefit and fee schedule (medical or behavioral health).
12)
How do ABA specialists bill under the new contract/fee schedule?
For Applied Behavioral Analysis (ABA) services, the following modifiers should be billed by these specialties:
- HP: Board Certified Behavior Analyst or Behavior Specialist Consultant (doctoral level)
- HO: Board Certified Behavior Analyst or Behavior Specialist Consultant, or Mobile Therapist (master's level)
- HN: Board Certified Assistant Behavior Analyst (bachelor's level)
- HM: Certified Support Staff or Therapeutic Staff Support (less than bachelor's level)
Contracting
13) How do I join the AmeriHealth Behavioral Health network if I have not received a new contract?
You can email
AmeriHealthBH@amerihealth.com to inquire about the status of your contract. Participating providers must provide your practice TIN, practice NPI (National Provider Identifier) and the name and email of the authorized signatory for the practice. Additional information may be required to join the network.
Note for group practices: Please ensure that your practitioner roster is up-to-date with Magellan. This will provide for a more seamless transfer of your practice practitioner demographics.
You will receive the contract to sign electronically via DocuSign which will contain three attachments: (1) letter describing the change, (2) contract requiring signature, and (3) prevailing fee schedule.
All NPIs for your practice should be included on the contract.
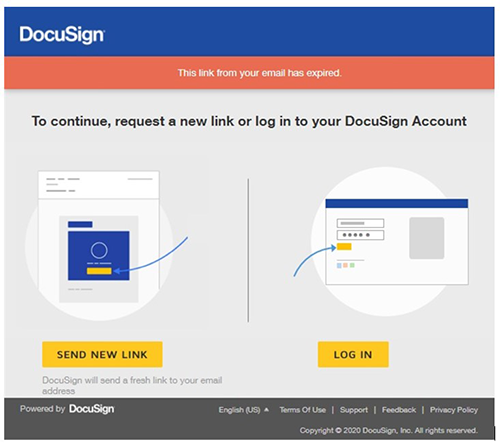
14) How do I resolve an expired DocuSign email?
The links in the contracts we send expire for security purposes. However, you can request a new link using the expired email.
Sign into DocuSign, then just click “send new link." Each time you click on the expired email link, DocuSign will send you a new email containing a fresh link.
15)
How does the new contract affect my practice since I/we already participate with Magellan?
Signing new AmeriHealth contracts will ensure you remain a participating provider with us effective January 1, 2023. As of this date, it will also transition your practice to the AmeriHealth prevailing fee schedule for services furnished to AmeriHealth members.
Signing a contract with AmeriHealth does not change or impact your status with Magellan. However, it is important to update your group practice roster with Magellan in order to ensure all practitioner information is seamlessly transferred by the January 1, 2023 effective date.
16)
What if I have questions or concerns regarding my current contract or fee schedule?
Since your current contract is with Magellan, please contact them directly:
www.MagellanProvider.com or 1-800-788-4005.
17)
What if a new clinician joins our practice?
Do they need to sign a contract, or can they be added to our January 1, 23 contract?
AmeriHealth contracts with the group practice, who in turn employs the practitioners/clinicians. AmeriHealth credentials each new practitioner and links the practitioner to the group practice. If the new practitioner is already credentialed, they simply need to be linked to your group.
AmeriHealth contracts directly with individual practitioners in a solo practice
18)
I keep seeing references to a group practice. What if I am a solo practitioner that wants to contract?
We welcome solo practitioners. A solo practitioner may sign their own individual contract.
Credentialing
19) I do not currently participate with Magellan or AmeriHealth. How do I get credentialed for 2023?
After your group or solo practitioner practice has signed a contract, you must complete a credentialling application with us for
AmeriHealth New Jersey or
AmeriHealth Pennsylvania if you do not currently participate with Magellan.
For 2022 credentialing, please contact Magellan.
After January 1, 2023, you will need to be credentialed by AmeriHealth and Magellan separately to participate in both networks.
20) Can I oversee and bill for clinicians who are under my direct supervision, but not credentialed (such as those who are in training, but not yet licensed, as well as other master's level clinicians)?
AmeriHealth maintains the highest level of accreditation standards, which require that all rendering practitioners be individually credentialed to treat our members. In addition, all professionals must hold a current license in their specialty in the state in which they practice, including telemedicine services.
Please refer to current Magellan credentialing criteria, which we expect will remain the same when AmeriHealth transitions to the direct network on January 1, 2023:
https://www.magellanprovider.com/media/11915/b_indivcrit.pdf
21) My practice is contracted with Magellan. How do I add or remove clinicians who have left?
All updates to your practice, including the individual clinician list, should be made via
www.MagellanProvider.com. If you signed a January 1, 2023 contract with AmeriHealth, these updates will transfer, so please ensure that your roster is up-to-date with Magellan.
Practitioners who maintain credentials with Magellan and whose practice signed a direct contract with AmeriHealth will remain a part of our network until recredentialing is required. You do not have to credential with us again until that time.
Claims
22) Will this change impact claim submissions or claim processing?
No. Claim processing will remain the same, since your claims are currently processed by AmeriHealth. However, the payment rates will change in accordance with the fee schedule tied to the 2023 contract.
23) Are we required to submit claims electronically and/or maintain electronic medical records?
All providers are encouraged to submit claims electronically. You can use our PEAR portal to submit 1500 claims, review claim status, and perform claim investigations. Submitting claims electronically and utilizing electronic medical records speeds up your payment and leads to better accuracy.
However, if you are a small practice with limited technology, we will work with you on navigating our claim submission process.
24)
Is there someone I can contact regarding claim submissions?
We encourage providers to use all of our self-service tools, which are available in the PEAR portal. Also, claims resources can be found on our provider website for
AmeriHealth New Jersey and
AmeriHealth Pennsylvania.
If you have additional questions or concerns, please call:
- AmeriHealth New Jersey: 1-888-YOUR-AH1 (1-888-968-7241)
- AmeriHealth Pennsylvania:1-800-275-2583
CPT Copyright 2017 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.