As we prepare to transition the last set of members in group plans to our new operating platform on July 1, 2025, we want to remind you of the importance of using the correct member ID number for the noted date of service.
Member ID cards
-
Newly issued member ID cards will have the new number structure (10-digit format). The new ID number will be at the member level, not the subscriber level, meaning each member will have a unique ID number.
-
It is important to ask members for a copy of their latest ID card at every visit to ensure proper claims processing.
-
To ensure you are viewing accurate information for the noted date of service, use the Eligibility & Benefits transaction on the Practice Management application of the Provider Engagement, Analytics & Reporting (PEAR) portal. For the most accurate results for the noted date of service, search for the member using their name and date of birth.
-
For providers who use the 270/271 transactions via the Electronic Data Interchange (EDI), here is an example* of the response you may see:
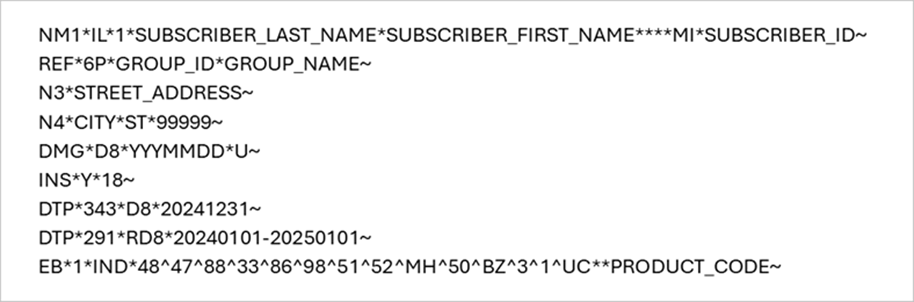
*The example is just a sampling of the response. The full response provides more detailed information on specific benefits, member cost-share for each type of service, and capitated providers, if applicable.
Authorizations
- Members who have a new ID number (10-digit format) may have an existing authorization that was submitted under their old ID number (12-digit UMI). Authorizations submitted under the member's old ID number remain valid.
You do not need to enter a new authorization under the member's new ID number.
Referrals
- Members who have a new ID number (10-digit format) may have an existing referral that was submitted under their old ID number (12-digit UMI). Referrals submitted under the member's old ID number remain valid.
You do not need to enter a new referral under the member's new ID number.
- When performing a Referral Search using the referral number, you may see two results — one with the old member ID number and the other with the new member ID number.
Claim submissions
- Claims will be processed based on the member's ID number on the date of service or date of admission. You do not need to split claims.
- Use the Eligibility & Benefits transaction in Practice Management to confirm the member ID number for each date of service to be billed.
- Claims submitted with an old ID number after the new card is effective will be denied with this message: “Member did not have eligible coverage." If this occurs, please obtain the new ID number from the member and submit a new claim. Please do not submit as a corrected claim.
- Use the payer ID grids to assist with claims submission instructions. Note that you may see multiple prefixes for some plans until the platform transition is complete.
Stay informed
Visit our dedicated
Platform Transition page for the latest news and FAQ related to the transition.
25-0024