Page Content QIPS ResourcesQIPS is Independence Blue Cross's value-based program for primary care practices. Eligible practices can earn financial incentives for providing quality health care and effectively managing the care of their HMO and PPO members, as well as BlueCard® PPO members. Population Health Specialists (PHS) are assigned to each practice and can assist you in improving QIPS performance and overall patient health outcomes.
 | | Updates | Due today! QPM score program electronic feedback - NEW! | 5/24/2023 | Today, May 24, 2023, is the last day for practices to submit their electronic feedback for the QPM score program for measurement year 2022. If you have not done so and wish to submit feedback, please access the QPM Feedback application from the PEAR portal. Key reminders - By completing feedback, your practice has a chance to improve its final results, which can positively impact your incentive amount.
- Once complete, each eligible form must be attested by an authorized user. Forms that result in the “Reviewed; No action required" status for all of a member's open care gaps do not require attestation.
If you have questions, please email Jennifer Kennedy.
|  |  | | Updates | One week left to complete your QPM score program electronic feedback – Due May 24 - NEW! | 5/17/2023 | The deadline to complete electronic feedback for the Quality Performance Measure (QPM) score program for measurement year 2022 is May 24, 2023. Please take time to complete your patient records before the deadline to ensure they are counted for feedback. Reminders - A patient record will only count towards feedback when it is marked as Complete. If a record status is Ready to Attest, the information will not be reviewed and counted.
- Use the “Reviewed (No action required)" button to confirm that the member's form was reviewed and there are no specific measures to complete as no service was performed. This option does not require provider attestation.
If you have questions, please email Jennifer Kennedy.
|  |  | | Updates | Extended! The deadline to complete your QPM score program electronic feedback is now May 24 - NEW! | 5/10/2023 | Independence Blue Cross is extending the deadline to complete electronic feedback for the Quality Performance Measure (QPM) score program for measurement year 2022. We received reports of performance issues within the QPM Feedback application, and a fix was applied to enhance the system responsiveness. In response, we are providing more time to complete and submit your feedback. The new deadline is Wednesday, May 24, 2023. Reminders - A patient record will only count towards feedback when it is marked as Complete. If a record status is Ready to Attest, the information will not be reviewed and counted.
- Use the “Reviewed (No action required)" button to confirm that the member's form was reviewed and there are no specific measures to complete as no service was performed. This option does not require provider attestation.
For help with the feedback process, review the QPM Feedback Application user guide, available on the PEAR Help Center under Analytics & Reporting – QIPS/Stars Programs.
If you have questions, please email Jennifer Kennedy.
|  |  | | Updates | Measurement year 2022 QPM score program electronic feedback is now live through May 17, 2023 - NEW! | 4/17/2023 | The following are available for the QPM score program for measurement year 2022: - QPM Feedback application. Log in to the PEAR portal and select the QPM Feedback application. You can review and complete the electronic forms for your patients for whom we do not have a record of receiving the indicated preventive service. Review the Instructions and Definitions section before reviewing and filling out the patient records.
- Updated QPM user guide. The updated QPM Feedback Application user guide is available on the PEAR Help Center to assist you in navigating the tool and completing the feedback forms.
- QPM Preliminary score report. Reports will be posted shortly. To view and download your preliminary report, select the PEAR Analytics & Reporting application, and then select Output Manager from the top navigation menu. The report will be under Published Reports.
Updates to QPM feedback application - “Reviewed (No action required)" button was added at the member level. This can be used to confirm that the member's form was reviewed and there are no specific measures to complete as no service was performed. This option does not require provider attestation.
- New column shows the number of open care gaps per member with hover text that lists each of the measures.
- Ability to select ALL when selecting your practice/entity. This allows you to view all of your open care gaps for all of your locations.
- “Patient Deceased Date" field was added to capture the date if the “Patient deceased" option was selected.
- “Absence of cervix" was added as a drop-down option for the cervical cancer screening measure.
- New diabetic measure added:
- Kidney Health Evaluation was added to the list of quality measures eligible for feedback.
Attestation process Once complete, each eligible form must be attested by an authorized user. As noted above, forms that result in the “Reviewed; No action required" status for all of a member's open care gaps, do not require attestation. If you have any questions, please contact Jennifer Kennedy.
|  |  | | Updates | QPM feedback process begins next week - NEW! | 4/11/2023 | The feedback process for the Quality Performance Measure (QPM) score program for measurement year 2022 begins next week.
- April 17, 2023:
- An email will be sent to announce launch of QPM Feedback application and will include program changes and new features. An updated QPM feedback user guide will be available as a resource on the PEAR Help Center.
- The QPM Preliminary reports available for review and download under Output Manager in the Analytics & Reporting application of the Provider Engagement, Analytics & Reporting (PEAR) portal.
- May 17, 2023: Last day to attest and submit electronic feedback forms.
Attestation process Although supporting documentation is not required when submitting feedback, forms must be attested by an authorized user for the feedback forms to be accepted. However, if a member's form status results in “Reviewed; No action required" for all of their open care gaps, attestation is not required in this scenario. If you have not done so already, consult with your PEAR Organization or Location Administrator to review the list of physicians who require attestation access and have them follow these steps to add or remove physicians as needed: - Log in to PEAR and select Provider Administration Tool.
- View each physician's PEAR profile by clicking the three dots under the Actions column. Note for Health Systems or provider groups: Please ensure that the physician who is to attest for each practice is credentialed at each practice location.
- Check to ensure they have a Clinical role for Analytics & Reporting for each practice and that the user's individual practitioner NPI is entered in their profile (if applicable).
If you have questions about the feedback process or your attesting physicians, please send an email to feedback@ibx.com. If you have general questions about the QIPS program, please contact Jennifer Kennedy.
|  |  | | Updates | QPM feedback process starts soon - NEW! | 3/22/2023 | The electronic feedback process will soon begin for measurement year 2022. Below is some information to help you get ready. We've also made updates to the tool to further improve your experience and reduce the administrative burden. IMPORTANT: Review your attesting physicians As with last year, physicians must attest that the information entered in the feedback forms is accurate to be accepted. A form is not considered complete until a physician completes the attestation. To ensure a successful workflow, consult with your PEAR Organization or Location Administrator to review the list of physicians who require attestation access and have them follow these steps to add or remove physicians as needed: - Log in to PEAR and select Provider Administration Tool.
- View each physician's PEAR profile by clicking the three dots under the Actions column. NOTE for Health Systems or provider groups: Please ensure that the physician who is to attest for each practice is credentialed at each practice location.
- Check to ensure they have a Clinical role for Analytics & Reporting for each practice location and that the user's individual practitioner NPI is entered in their profile (if applicable).
Please complete your review and make any necessary changes by April 1, 2023. If you have questions about this process or your attesting physicians, please send an email to feedback@ibx.com.
Key updates to QPM feedback application - “Reviewed (No action required)" button was added at the member level. This can be used to confirm that the member's form was reviewed, but there are no specific measures to complete as no service was performed.
- “Patient Deceased Date" field was added to capture the date if the “Patient deceased" option was selected.
- New measure added: Kidney Health Evaluation was added to the list of quality measures eligible for feedback.
Feedback timeline The QPM feedback application will be available in mid-April on the PEAR portal and will be open for one month. Specific dates and more detail will be provided in early April. An updated user guide explaining how to access, complete, and attest to the feedback forms will be available on the PEAR Help Center at that time. In the meantime, we encourage you to review the details of the QPM score program, as well as the overall QIPS program, in the QIPS Program Manual – Measurement year 2022. If you have questions, please contact Jennifer Kennedy.
|  |  | | Updates | DID YOU KNOW? - NEW! | 3/22/2023 | A new measure was introduced into the QPM score program for MY 2023 called Primary Care Visit. This measure evaluates the percentage of your Medicare Advantage members who visited a PCP within the measurement year. What you need to know Review the Primary Care Visit measure details. Is there a report in PEAR AR to help me with this measure? Yes, the Members with No Recorded PCP Visits – Practice report shows your Medicare Advantage members who have not been seen in the past 12 months. It includes all Medicare Advantage members regardless of chronic condition status. Commercial members are also included if they have not been seen in the last 12 months AND have a chronic condition. Use this report to help identify your Medicare Advantage patients who have NOT been seen in the past 12 months for the purposes of the Primary Care Visit measure. Schedule each patient for a visit within the measurement year (2023). This will help you reach the Primary Care Visit QPM band level you would like to achieve.
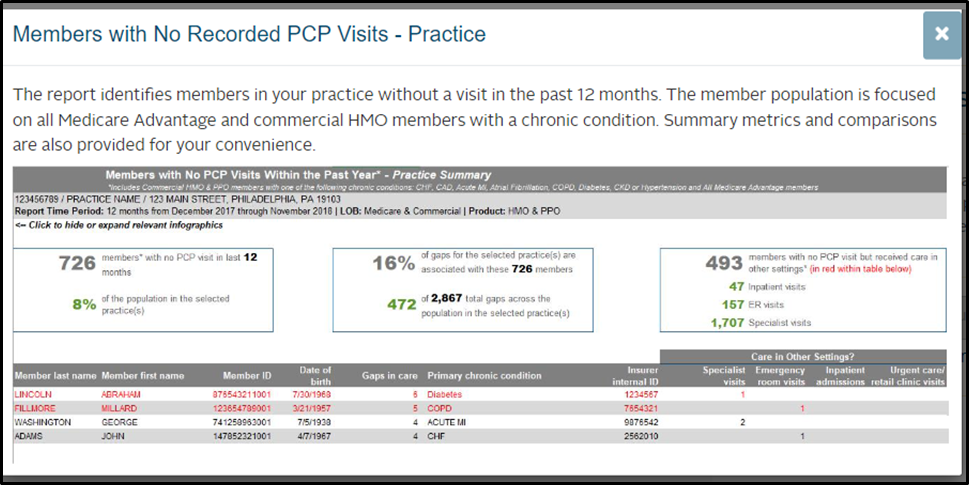
How do I access this report? - Log into the PEAR portal and select PEAR AR.
- Select Report Center from the top navigation bar, and then select Population Health Reporting.
- Select your practice(s).
- Select the report option: Members with no Recorded PCP visits – Practice.
If you have more questions on this measure, please contact your assigned Population Health Specialist or email Jennifer Kennedy.
|  |  | | Updates | Updated targets for medication management - NEW! | 3/14/2023 | We discovered an error in the QIPS Program Guide – measurement year 2023. The targets displayed in Section 5 for the Medication Management measure, included in the Quality Performance Measure (QPM) score program, were not updated according to the Centers for Medicare & Medicaid Services (CMS) and National Committee for Quality Assurance (NCQA) national ratings. The Medication Management measure consists of: - Medication adherence for high cholesterol, high blood pressure, and/or diabetes medications; and
- Statin dispensed based on disease prevalence.
The targets currently displayed in the QIPS program guide are as follows:
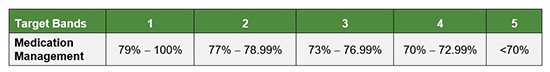
Updated targets We adjusted the targets to reflect a weighted average of the CMS and NCQA benchmarks for Commercial and Medicare Advantage triple-weighted populations. Please see the updated targets below:
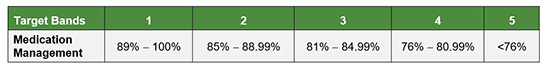
We will update the QIPS Program Guide – measurement year 2023 and the PEAR Analytics & Reporting financial dashboard to reflect the new targets within 30 days. Because Medication Management is a new quality measure for measurement year 2023, it will not be assessed for the Improvement Incentive. If you have questions, please contact Jennifer Kennedy.
|  |  | | Updates | Updated age for colorectal cancer screening - NEW! | 1/18/2023 | In 2021, the U.S. Preventive Services Task Force updated the recommended age to begin screening for colorectal cancer to age 45. The Independence Blue Cross (Independence) preventive services medical policy was updated September 1, 2021, to reflect this change. In addition, the Independence QIPS program has been updated to reflect the new age recommendation for colorectal cancer. The QIPS program guide for measurement year 2023 has been updated to reflect the new age recommendation. The Gaps in Care report, available via PEAR Analytics & Reporting, will be updated in February. In addition, the colorectal cancer screening targets will be reviewed and adjusted this summer to reflect the new age change. Check this page periodically for program updates throughout the year. Please contact Jennifer Kennedy with any questions.
|  |  | | Updates | New resource for the Rx Adherence and Usage report - NEW! | 10/20/2022 | A new guide is available that provides best practices for reviewing the Rx Adherence and Usage report on the PEAR Portal, in PEAR AR (Analytics & Reporting). It shows you how to incorporate this information into your organization's workflow, to assist members who are eligible for the medication adherence measures in our QIPS program and Medicare's Five-Star Quality Rating Program (Stars Program). You can find the guide in the PEAR Help Center under Analytics & Reporting – QIPS/Stars Programs.
|  |  | | Updates | Top quality recognition - NEW! | 10/18/2022 | Independence Blue Cross congratulates these primary care offices for achieving top quality practice recognition in the Quality Performance Measure (QPM) score program. These offices achieved a mean band of less than or equal to 2.5 and had no quality measures resulting in the lowest band (band 5) and at least one quality measure in the highest band (band 1) in the QPM score program, a component of the Quality Incentive Payment System (QIPS) program, for measurement year 2021. You can find details of the QPM score program, including the measures scored, in the QIPS Manual – measurement year 2021.
|  |  | | Updates | Opt in now to the QIPS program for MY2023 - NEW! | 10/4/2022 | It's time to opt in for QIPS measurement year (MY) 2023! Primary care practices may start submitting requests to participate in the Quality Incentive Payment System (QIPS) program. Highlights of changes for MY2023 - You must complete the Satisfaction Survey on the PEAR portal prior to opting in. We encourage all personnel (clinical and administrative staff) to complete the survey so we can collect well-rounded feedback from your practice.
- For the adult programs:
- We added a new quality measure, Primary Care Visit (Medicare Advantage), to the Quality Performance Measure (QPM) score program.
- We increased payments for the Improvement incentive, Engagement incentive, and QPM Band 1 and Band 2.
- We added an additional component for the Transitions of Care incentive (Medicare Advantage): Follow-up after ED visit for members with multiple high-risk chronic conditions.
How to opt in The deadline to complete the opt-in process is January 6, 2023. Use the Analytics & Reporting (AR) application on the PEAR portal to complete the opt-in process. Practices that do not opt in to the QIPS program by the deadline will not be included in the program or be eligible to earn incentive payments for measurement year 2023. Practices that opted in for measurement year 2022 still need to complete the process for measurement year 2023. Please review and affirm or correct pre-populated information as you complete the opt-in process. Review these resources to help you during the opt-in process: If you did not opt in to the QIPS program for measurement year 2022, you will be asked to identify an Office Champion and a Clinical Champion. TIP: Identify the Office and Clinical Champions before you begin for a smoother process. For more information regarding the QIPS opt-in process, please email Jennifer Dombrowski.
If your question is of a clinical nature, please contact Ellen Riccobene, M.D.
|  |  | | Updates | QIPS program results and program changes | 8/18/2022 | We recently completed our review and calculated the results for the Quality Incentive Payment System (QIPS) program for measurement year 2021. As we assessed the preliminary performance and post-feedback results for measurement year 2021, we determined that some additional changes to the QIPS program were needed. Program changes The following changes will be made as a result of our review of the 2021 program performance. The QIPS manuals will be updated to reflect these changes and will be available on the Value-based programs page. - Measurement year 2021:
- Mean band. Due to impacts of the COVID-19 pandemic, we saw lower than anticipated performance in certain quality measures. Therefore, we have adjusted the mean band threshold from 2.5 to 3.0 to ensure practices are not unfairly disqualified for the Cost & Care Efficiency measures.
- Pediatric immunization targets. We realized that our original targets were set too high and were a bit too aggressive at this time. Therefore, the targets have been adjusted.
- Measurement year 2022:
- Diabetic care combination. We heard your feedback, and we will be unbundling the diabetic care measures. Eligible members will no longer need to meet all three metrics to receive credit for being compliant. Each metric will be treated as a separate quality measure and will be rolled into a new diabetic care combination, giving practices credit for each metric achieved.
- Pediatric immunization targets. The measurement year 2021 changes to the targets will be carried forward into measurement year 2022.
2021 program payments and report Payments for measurement year 2021 will be made in the coming weeks. You can use the QIPS Payment Roster in PEAR Analytics & Reporting (AR) to view a member-level breakdown of these payments. For help finding the information, please refer to the Accessing QIPS payment rosters from the report center video in the PEAR Help Center. Your final report will also be available soon in PEAR AR by selecting Output Manager at the top of the page, then Published Reports. We have consolidated all program results into one final report for your convenience. The report now contains your QIPS overall results and your QPM score program performance.
|  |  | | Updates | Revised Practice Financial Dashboard | 8/10/2022 | We recently made changes to the presentation and data available in the Practice Financial Dashboard within the PEAR Analytics & Reporting application to make it easier to review your financial performance. Earnings Summary: - Data now displays for the current year and prior two years.
- Payment types are presented in stacked bar charts. You can hover over each section to view the specific category totals.
- The payment types are arranged alphabetically and align with the descriptions presented in the transaction registry. The registry remains segmented by category and check number.
Transaction registry: - View payments by month and check number for each of the measures/payment types that are presented in the bar charts.
- Certain measures will pay across multiple checks for payments driven by membership plans.
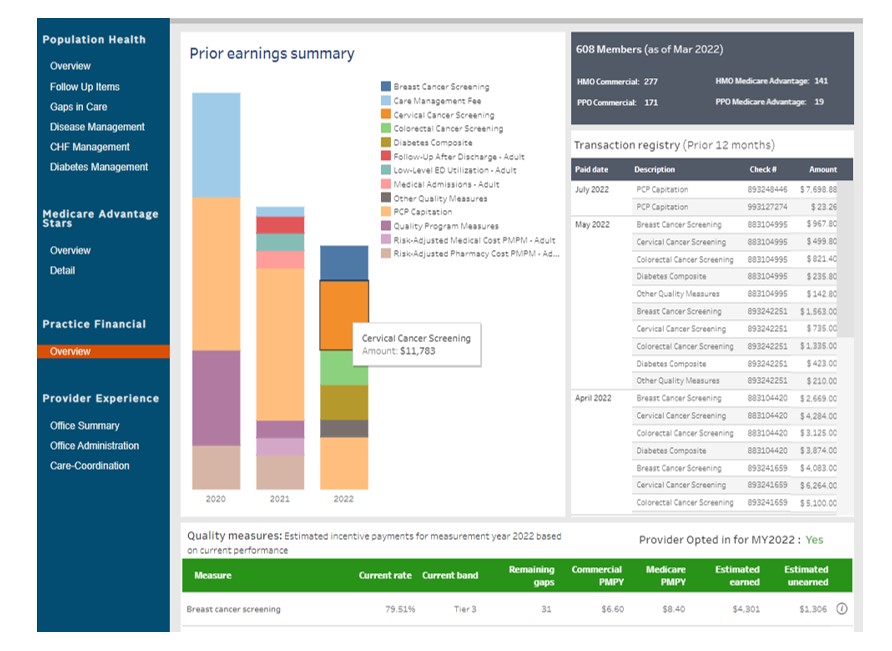
Quality measures: - Your current QIPS opt-in status is clearly displayed.
- Three new columns have been added: Current rate, Current band, and Remaining gaps.
- The Current rate and Current band columns contain the same information that was previously presented as hover text.
- The Remaining gaps column represents the number of members currently required to come into compliance to improve to the next band.
|  |  | | Updates | QPM alert: Closing Medication Reconciliation care gaps | 7/12/2022 | Our data shows a concerning amount of open care gaps for Medication Reconciliation after patients are discharged from inpatient settings. While our data shows that patients are being seen for post-hospitalization follow-up, it also shows more open Medication Reconciliation care gaps. If both of these pieces are not complete, this could negatively affect your Transitions of Care (TRC) QIPS incentive performance. One of the following may be occurring for Medication Reconciliation: - The medications are being reconciled post-discharge, but the appropriate coding is not taking place. Reference the table below for appropriate Medication Reconciliation codes.
- The medications are not being reconciled post-discharge. They should be reviewed during the patient visit, and appropriate coding should take place.
How to identify members - Access PEAR Analytics & Reporting
- Under Population Health, select “Follow Up Items"

- Navigate to “Recently Discharged Patients - within last 14 days"
- A member roster will appear. Leverage the “i" icon for more information about the discharge.
What is needed to be compliant for TRC TRC evaluates the percentage of members who are 18 and older and had each of the following: - Notification of Inpatient Admission: Members who had documentation of notification of inpatient admission on the day of admission through 2 days after the admission.
- Receipt of Discharge Information: Members who had documentation of discharge information on the day of discharge through 2 days after the discharge.
- Patient Engagement After Inpatient Discharge: Members who had a form of patient engagement (office visit, visits to the home, telehealth) provided within 30 days after discharge. (QIPS)
- Medication Reconciliation Post-Discharge: Members who had documentation of medication reconciliation on the date of discharge through 30 days after discharge. (QIPS)
How to close the care gap 1. Patient Engagement Code: See section 1 below. -AND- 2. Medication Reconciliation Code: See section 2 below. -THEN- 3. Submit a claim/encounter with appropriate coding from the below tables. Note: If the discharge is followed by a readmission or direct transfer to an acute or nonacute inpatient care setting on the date of discharge through 30 days after discharge (31 days total), use the admit date from the first admission and the discharge date from the last discharge. 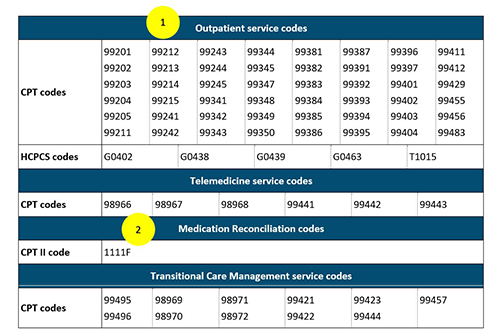
Resubmission of claims A corrected claim can be submitted to include the Medication Reconciliation code. This is only applicable when the appropriate medication reconciliation took place during a patient follow-up visit. Please refer to the Claim investigation and corrected claim submission procedures article for further information. Need help? Access the Gap Closures Guide on the PEAR Help Center to learn more about closing care gaps for the TRC measure.
|  |  | | Updates | New measures added to QIPS for MY2022 | 2/21/2022 | Two new measures have been added to QIPS for MY2022 – Controlling Blood Pressure and Kidney Health Evaluation. Please refer to the Gap Closures Guide to learn more about closing these gaps in care. Controlling blood pressure (CBP) This measure evaluates the percentage of members ages 18 through 85 who had a diagnosis of hypertension (HTN) and whose blood pressure (BP) was adequately controlled (<140/90 mm Hg) during 2022. - Denominator. Commercial and Medicare Advantage members ages 18 through 85 as of December 31, 2022.
- Numerator. The most recent BP reading during 2022 on or after the second diagnosis of HTN. If no BP is recorded during the measurement year, the member's BP is assumed to be out of control.
Kidney Health Evaluation for Patients with Diabetes (KED) This measure evaluates the percentage of members ages 18 through 85 with diabetes (Type 1 and Type 2) who received a kidney health evaluation, defined by an estimated glomerular filtration rate (eGFR) and a urine albumin creatinine ratio (uACR). - Denominator. Commercial and Medicare Advantage members with diabetes (Type 1 and/or Type 2) who are ages 18 through 85 as of December 31, 2022. There are two ways to identify members with diabetes: by claim/encounter data and by pharmacy data.
- Numerator. Members who received both an eGFR and a uACR during the measurement year on the same or different dates of service:
- At least one estimated glomerular filtration rate (eGFR) test.
- At least one urine albumin creatinine ration (uACR) test identified by either of the following:
- Both a quantitative urine albumin test and a urine creatinine test with service dates four days or less apart.
- A urine albumin creatinine ratio (uACR) test.
|  |
|
Follow javascript: SP.SOD.executeFunc('followingcommon.js', 'FollowDoc', function() { FollowDoc('{ListId}', {ItemId}); }); 0x0 0x0 ContentType 0x01 1100 Compliance Details javascript:if (typeof CalloutManager !== 'undefined' && Boolean(CalloutManager) && Boolean(CalloutManager.closeAll)) CalloutManager.closeAll(); commonShowModalDialog('{SiteUrl}'+
'/_layouts/15/itemexpiration.aspx'
+'?ID={ItemId}&List={ListId}', 'center:1;dialogHeight:500px;dialogWidth:500px;resizable:yes;status:no;location:no;menubar:no;help:no', function GotoPageAfterClose(pageid){if(pageid == 'hold') {STSNavigate(unescape(decodeURI('{SiteUrl}'))+
'/_layouts/15/hold.aspx'
+'?ID={ItemId}&List={ListId}'); return false;} if(pageid == 'audit') {STSNavigate(unescape(decodeURI('{SiteUrl}'))+
'/_layouts/15/Reporting.aspx'
+'?Category=Auditing&backtype=item&ID={ItemId}&List={ListId}'); return false;} if(pageid == 'config') {STSNavigate(unescape(decodeURI('{SiteUrl}'))+
'/_layouts/15/expirationconfig.aspx'
+'?ID={ItemId}&List={ListId}'); return false;}}, null); 0x0 0x1 ContentType 0x01 898 Document Set Version History /_layouts/15/images/versions.gif?rev=40 javascript:SP.UI.ModalDialog.ShowPopupDialog('{SiteUrl}'+
'/_layouts/15/DocSetVersions.aspx'
+ '?List={ListId}&ID={ItemId}') 0x0 0x0 ContentType 0x0120D520 330 Send To other location /_layouts/15/images/sendOtherLoc.gif?rev=40 javascript:GoToPage('{SiteUrl}' +
'/_layouts/15/docsetsend.aspx'
+ '?List={ListId}&ID={ItemId}') 0x0 0x0 ContentType 0x0120D520 350
MY2022
|
Measurement Year 2022
|
MY2023
|
Measurement Year 2023
|
PEAR
|
Provider Engagement, Analytics & Reporting
|
PEAR AR
|
PEAR Analytics & Reporting
|
QIPS
|
Quality Incentive Payment System
|
QPM
|
Quality Performance Measure
|
Suggestions? If you have topics you’d like covered in future posts, please contact Jennifer Kennedy.
|
|
Important Reminders |
MY 2022 QPM feedback window is now closed.
|
Adult Quality Measures for 2023
-
New: Primary Care Visit (Medicare Advantage members only) - This measure evaluates the percentage of your Medicare Advantage members who have visited a PCP within the measurement year.
- Update: Colorectal Cancer Screening - Age range updated from 51 to 75 to 45 to 75. Targets related to this change will be evaluated this summer.
QIPS Milestones
|
Opt-In
|
October to December
|
Engagement Incentive
|
Monthly payment & reviewed quarterly for meeting requirements
|
|
Preliminary Reports |
April
|
QPM Feedback Process
|
April - May
|
Final Reports & Payments
|
August
|
|